
Engaging men as contraceptive users: The time is now
A tool to support advocacy for the inclusion of vasectomy in family planning programs
Learn more
How to use this tool
The problem
“[Vasectomy] is for the benefit for everyone; it's for the benefit of the men, to the benefit of the women, to the benefit of the children, to the benefit of the nation.”
- Vasectomy service provider in Kenya
Vasectomy service benefits for men and couples
Vasectomy is a safe and effective method that offers benefits for individuals and heterosexual couples who know they do not want to have any or more children.






Vasectomy promotes the role of men as caring partners by allowing men to share responsibility for reproduction.
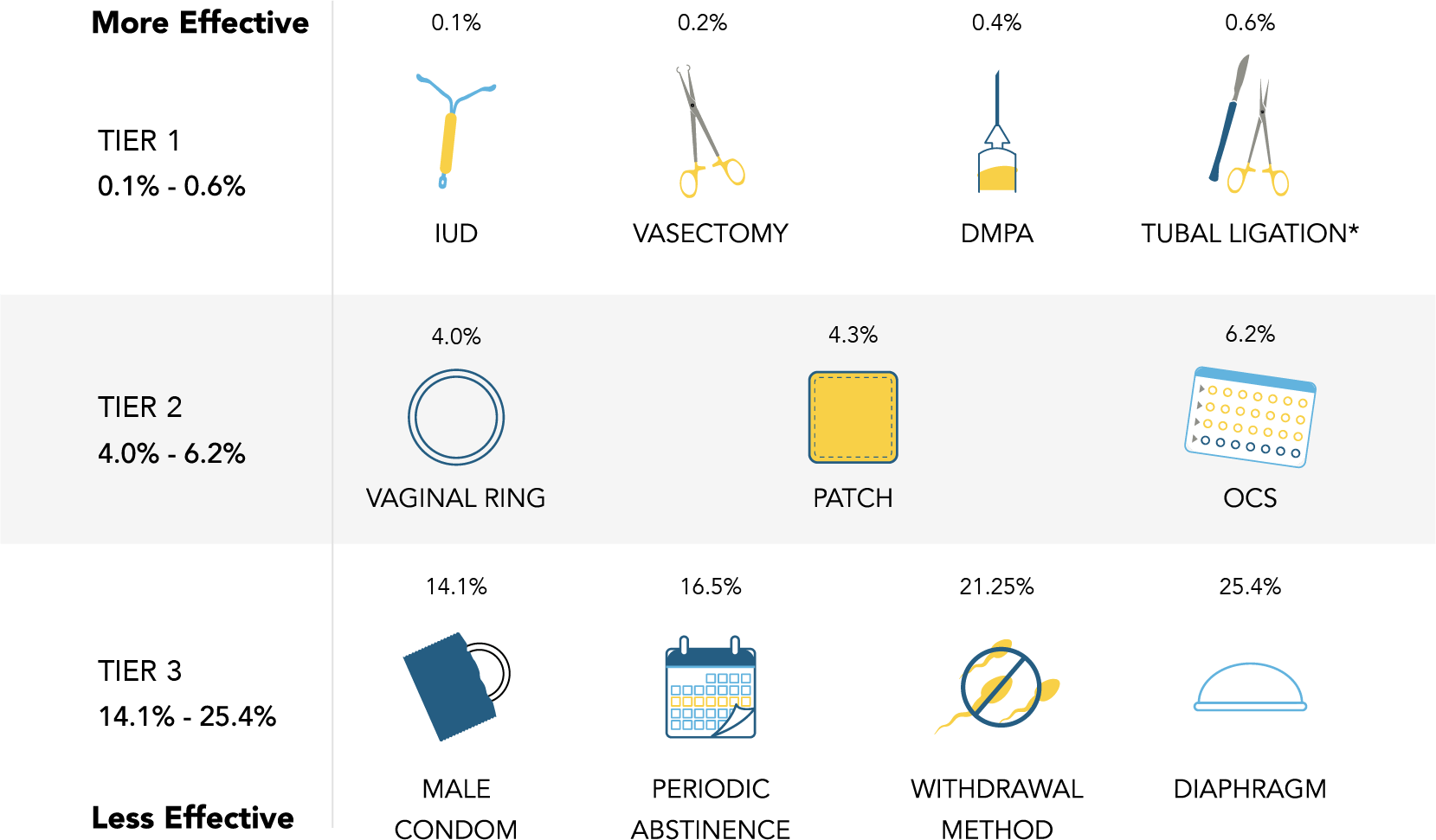
Vasectomy has a very low risk of complications or side effects. While tubal ligation is also considered very safe, it requires scalpel incisions, a longer recovery time, and general anesthesia, which carries greater risk.
Vasectomy does not require an extra step to prevent pregnancy before sex, like putting on a condom.*
Compared to tubal ligation, vasectomy is a quick procedure (< 30 minutes) and can be performed in an outpatient setting without anesthesia.
Social/relationship
Safety
2
2
Convenience
*After a vasectomy, couples should use another method of contraception until a doctor can confirm there is no sperm present in the semen. It is estimated to take three months and 15-20 ejaculations after the procedure before the semen is free of sperm.
3
Cost
Vasectomy is inexpensive compared to the cumulative cost of using shorter-term methods to limit births.
3
Ease
Vasectomy is over 99% effective in preventing pregnancy.
2,3
Effectiveness
2,3
In two thirds of FP2030 countries, less than 30% of the population has access to vasectomy.
4




Vasectomy program funding has been insufficient and inconsistent.


Vasectomy is unavailable
In roughly two thirds of FP2030 countries, less than 30% of the population has access to vasectomy.
Percent of the population with access to vasectomy in FP2030 countries
4

Vasectomy is underutilized
In sub-Saharan Africa, vasectomy accounts for less than 0.1% of contraceptive use.
Even where tubal ligation is common and accepted (i.e., Latin America, the Caribbean, and parts of Asia), vasectomy prevalence is low.
5

In sub-Saharan Africa, vasectomy accounts for less than 0.1% of contraceptive use.
5
Percent of contraceptive users using
a permanent method
Tubal ligation
Vasectomy
Latin America and the Caribbean
East and Southeast Asia
Central and South Asia
27.6%
2.2%
16.7%
1.5%
52.2%
1.0%
Vasectomy is underfunded
Vasectomy program funding has been insufficient and inconsistent.

A review of articles and program materials published between 2005 and 2015 found that these five USAID-funded cooperative agreements had vasectomy components:
Why should vasectomy be included in family planning programs?
Click to explore each key message below
Vasectomy is highly
cost-effective

Increasing access to vasectomy is critical to method choice

Demand for limiting births is high and
likely to rise

Vasectomy preserves women’s health and promotes gender equality

Evidence shows we can increase the demand for vasectomy

Expanding access to vasectomy sets the stage for future male methods in the future

Case studies
Nepal
Experience in Nepal demonstrates that mobile services can increase voluntary uptake of vasectomy.
Download the full case study
Rwanda
The PROGRESS project in Rwanda shows that demand for and uptake of vasectomy can increase with investment.
1. World Vasectomy Day. (2015). Vasectomy conversations #3 [video]. YouTube. Access this resource
2. Sharlip, I. D., Belker, A. M., Honig, S., Labrecque, M., Marmar, J. L., Ross, L. S., Sandlow, J. I., Sokal, D. C., & American Urological Association (2012). Vasectomy: AUA guideline. Journal of Urology, 188(6 Suppl), 2482–2491. Access this resource
3. Mayo Clinic. (2021). Vasectomy. Access this resource
4. Track 20. (2017). Availability of methods. Access this resource
5. United Nations, Department of Economic and Social Affairs, Population Division (2019). Contraceptive Use by Method 2019 [Data Booklet]. Access this resource
6. Perry, B., Packer, C., Chin Quee, D., Zan, T., Dulli, L., & Shattuck. D. (2016). Recent experience and lessons learned in vasectomy programming in low-resource settings: A document review. FHI 360. Access this resource
7. Sonnenberg, F. A., Burkman, R. T., Hagerty, C. G., Speroff, L., & Speroff, T. (2004). Costs and net health effects of contraceptive methods. Contraception, 69(6), 447-459. Access this resource
8. USAID. (2019). Couple years of protection (CYP). Access this resource
9. Tumlinson, K., Steiner, M. J., Rademacher, K. H., Olawo, A., Solomon, M., & Bratt, J. (2011). The promise of affordable implants: is cost recovery possible in Kenya? Contraception, 83(1), 88-93. Access this resource
10. Bertrand, J. T., Ross, J., Sullivan, T. M., Hardee, K., & Shelton, J. D. (2020). Contraceptive method mix: Updates and implications. Global Health: Science and Practice, 8(4), 666-679. Access this resource
11. Ross, J., & Stover, J. (2013). Use of modern contraception increases when more methods become available: analysis of evidence from 1982–2009. Global Health: Science and Practice, 1(2), 203-212. Access this resource
12. Department of Reproductive Health, World Health Organization. (2018). Family Planning Evidence Brief – Expanding contraceptive choice WHO/RHR/17.14 Rev.1. Access this resource
13. Wang, W., & Mallick, L. (2019). Understanding the relationship between family planning method choices and modern contraceptive use: An analysis of geographically linked population and health facilities data in Haiti. BMJ Global Health, 4(Suppl 5), e000765. Access this resource
Page 1 of 3
Next
14. United Nations Department of Economic and Social Affairs, Population Division (2020). World Fertility and Family Planning 2020: Highlights. Access this resource
15. Van Lith, L. M., Yahner, M., & Bakamjian, L. (2013). Women's growing desire to limit births in sub-Saharan Africa: meeting the challenge. Global Health: Science and Practice, 1(1), 97-107. Access this resource
16. Ahmed, S., Li, Q., Liu, L., & Tsui, A. O. (2012). Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet, 380(9837), 111-125. Access this resource
17. O'Loughlin, J. (1997), Safe motherhood: impossible dream or achievable reality? Medical Journal of Australia, 167: 622-625. Access this resource
18. International Planned Parenthood Federation. (2009). The truth about ... men, boys and sex: Gender transformative policies and programmes. Access this resource
19. Rottach, E., Schuler, S. R., & Hardee-Cleaveland, K. (2009). Gender perspectives improve reproductive health outcomes: New evidence. Population Reference Bureau. Access this resource
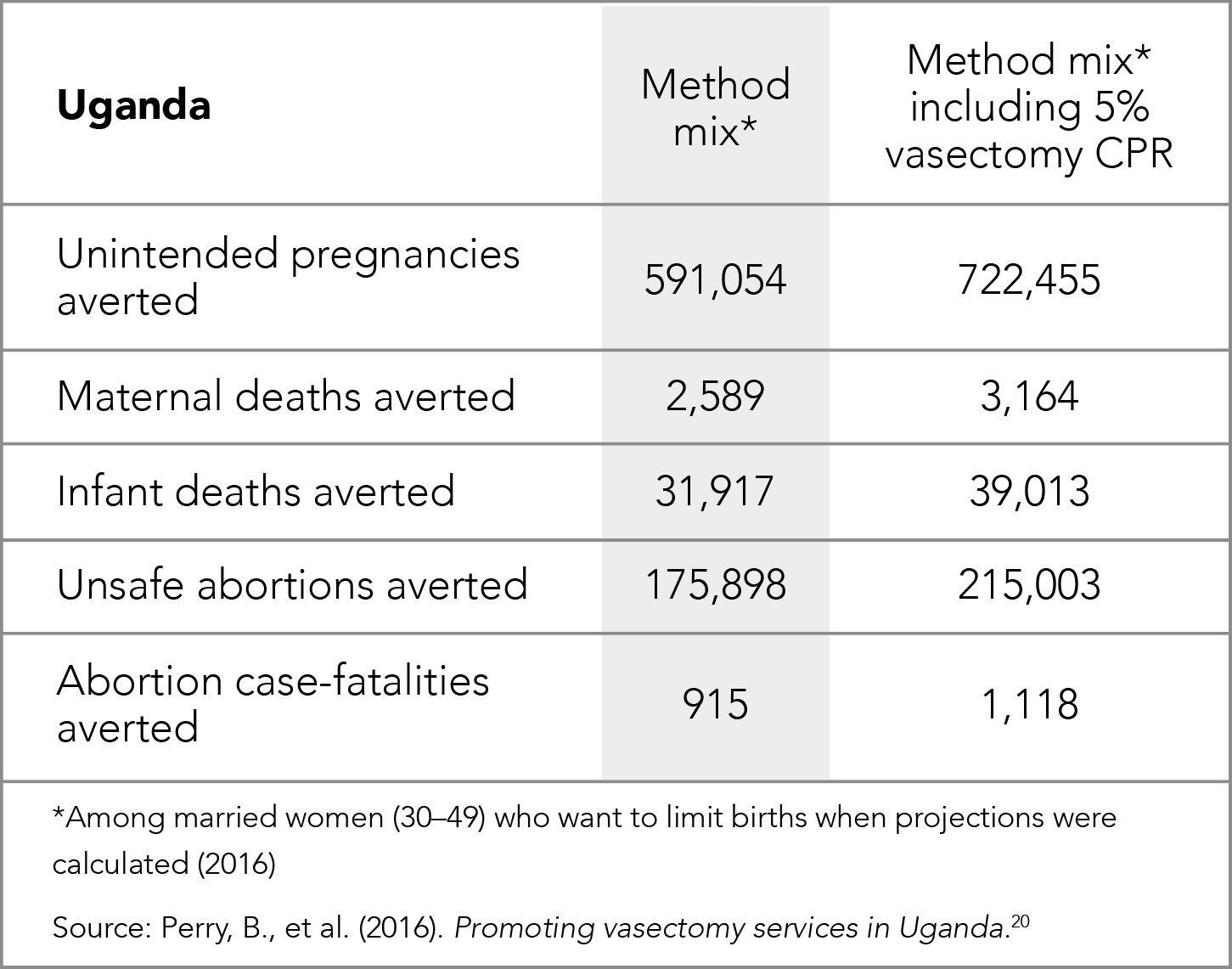
20. Perry, B., Packer, C., Chin-Quee, D., Zan, T., Shattuck, D. (2016). Promoting vasectomy services in Uganda. Durham, NC: FHI 360 and Washington, DC: The Population Council, the Evidence Project. Access this resource
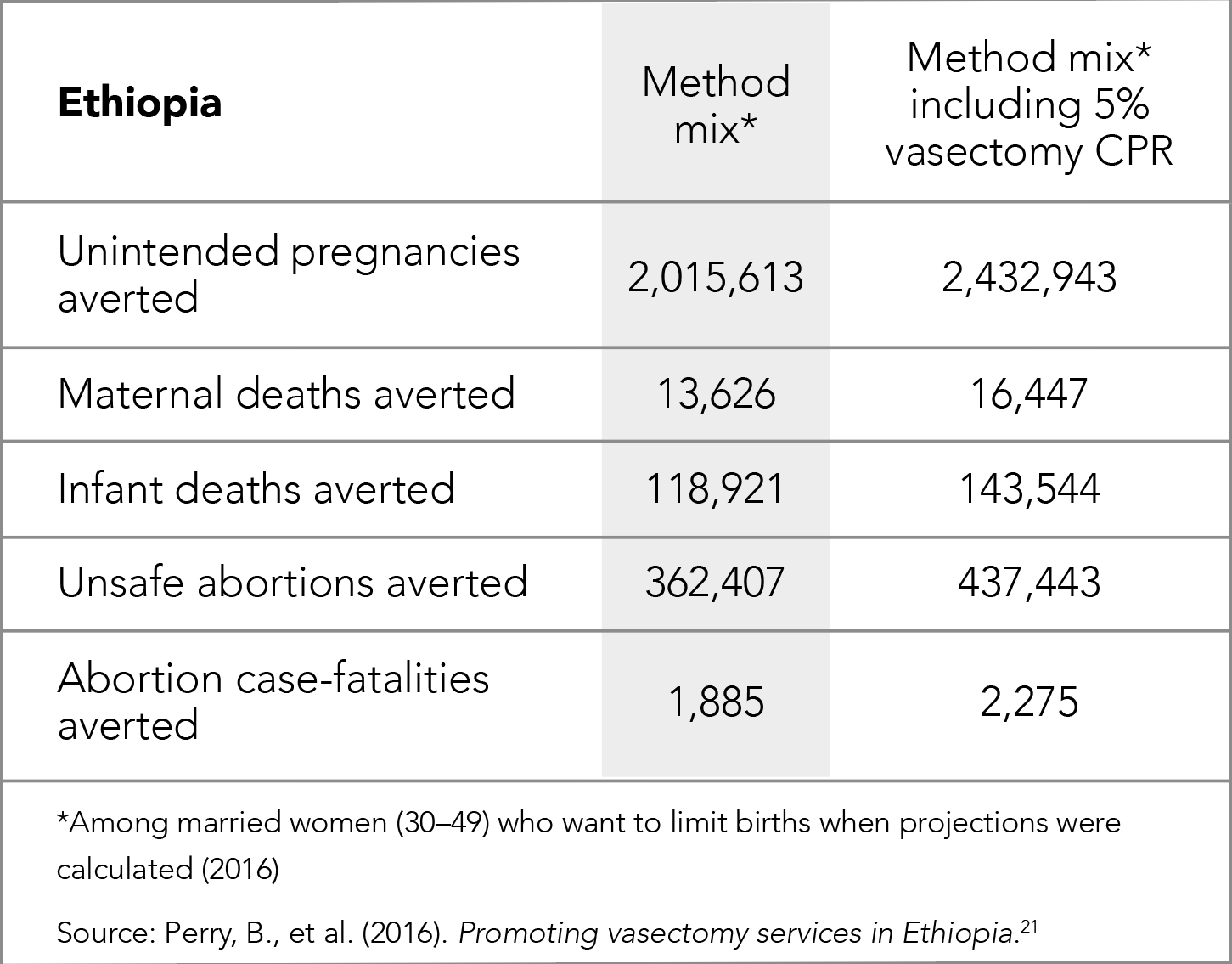
21. Perry, B., Packer, C., Chin-Quee, D., Zan, T., Shattuck, D. (2016). Promoting vasectomy services in Ethiopia. Durham, NC: FHI 360 and Washington, DC: The Population Council, the Evidence Project. Access this resource
22. Perry, B., Packer, C., Chin-Quee, D., Zan, T., Shattuck, D. (2016). Promoting vasectomy services in the Philippines. Durham, NC: FHI 360 and Washington, DC: The Population Council, the Evidence Project. Access this resource
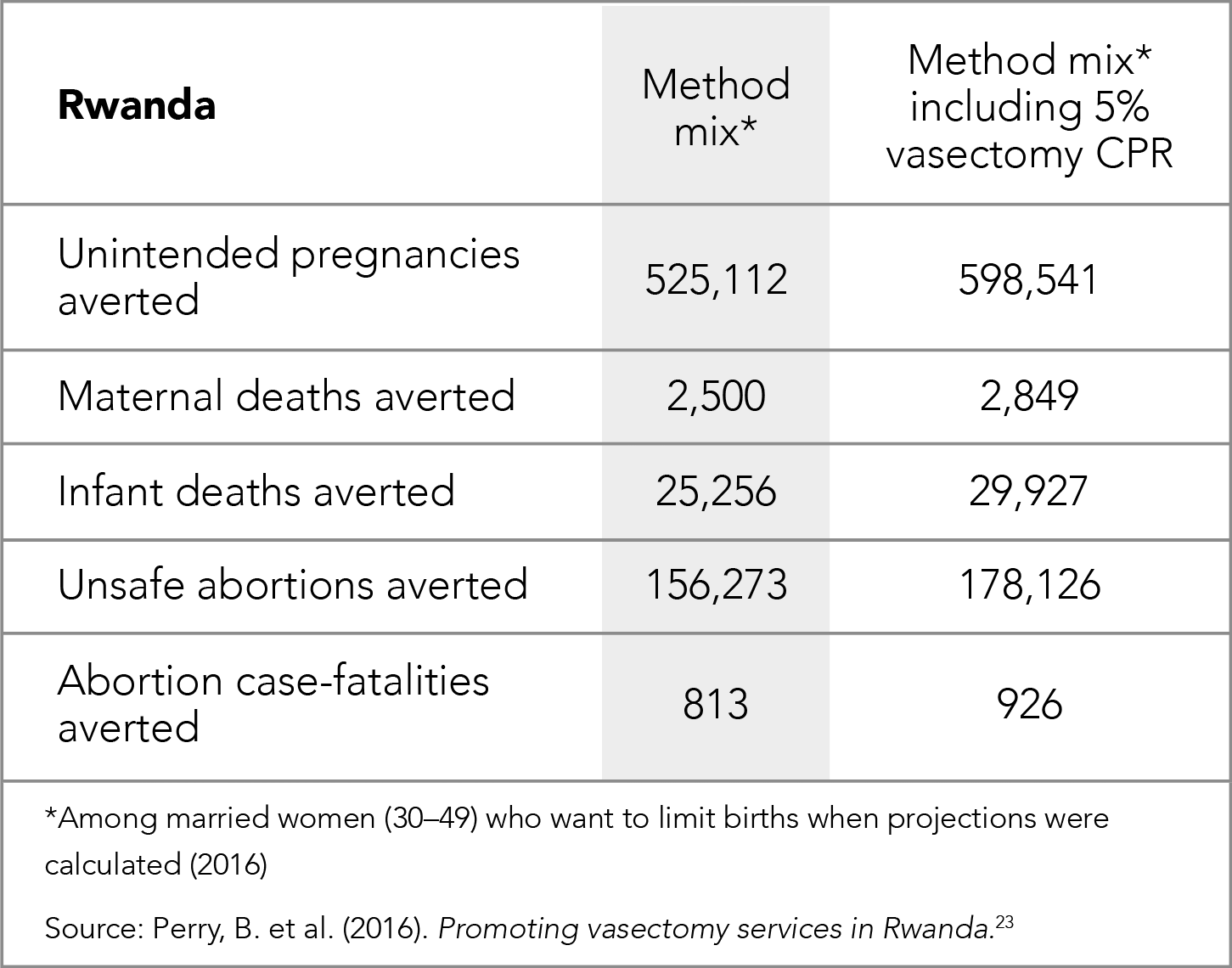
23. Perry, B., Packer, C., Chin-Quee, D., Zan, T., Shattuck, D. (2016). Promoting vasectomy services in Rwanda. Durham, NC: FHI 360 and Washington, DC: The Population Council, the Evidence Project. Access this resource
24. Shelton, J. D., & Jacobstein, R. (2016). Vasectomy: A long, slow haul to successful takeoff. Global Health: Science and Practice, 4(4), 514-517. Access this resource
Page 2 of 3
Previous
Next
25. Kincaid, D. L., Merritt, A. P., Nickerson, L., de Castro Buffington, S., De Castro, M. P. P., & De Castro, B. M. (1996). Impact of a mass media vasectomy promotion campaign in Brazil. International Family Planning Perspectives, 22(4), 169-175. Access this resource
26. Yahner, M., & Cisek, C. (2012). Using an employer-based approach to increase support for and provision of long-acting and permanent methods of contraception: The India experience. The RESPOND project study series: Contributions to global knowledge: Report no. 7. Access this resource
27. Knowledge SUCCESS. (2021). What works in family planning and reproductive health, part 1: Male engagement. Johns Hopkins Center for Communication Programs. Access this resource
28. David, F. P. (2003). Group counseling as an approach to family planning promotion and dropout reduction, with focus on no-scalpel vasectomy: An experimental trial and process documentation study. Iloilo City (Philippines): Social Science Research Institute, Central Philippine University. Access this resource
29. Subramanian, L., Cisek, C., Kanlisi, N., & Pile, J. M. (2010). The Ghana vasectomy initiative: Facilitating client–provider communication on no-scalpel vasectomy. Patient Education and Counseling, 81(3), 374-380. Access this resource
30. The ACQUIRE Project. (2005). “Get a permanent smile”—Increasing awareness of, access to, and utilization of vasectomy services in Ghana. EngenderHealth. Access this resource
31. Davis, J., de Vries, D.H., Sinzahera, J., Twahirwa, W., & Sokal, D.C. (2009). Final Feasibility Evaluation for No-Scalpel Vasectomy in Rwanda. Chapel Hill, NC: IntraHealth International, Capacity Project. Access this resource
32. FHI 360 & Rwandan Ministry of Health. (2011). Rwanda takes no scalpel vasectomy nationwide. FHI 360.
33. FHI 360. (2013). No-scalpel vasectomy: Scale-up. Approach in Rwanda shows promise. Research Triangle Park, NC: FHI 360. Access this resource
Page 3 of 3
Previous
references
Vasectomy is highly cost-effective
Vasectomy has the potential to generate significant health systems
cost-savings

Cost-effectiveness
Cost per CYP
7
Vasectomy is one of the most cost-effective methods of contraception
On average, vasectomy saves the U.S. healthcare system 9,936 USD per person over two years compared with no contraceptive use.
Method
Vasectomy
DMPA
Copper IUD
Cost savings vs.
no method (USD)
9,936
9,815
9,765
Health system cost savings from
contraceptive use after two years
Condom
OCs
Monthly injectable
Tubal ligation
No method
8,899
8,827
8,770
5,907
Source: Sonnenberg, F. A., et al. (2004). 69(6), 447-459.
Source: Tumlinson, K. et al. (2011). Contraception, 83(1), 88-93.
Service delivery costs per CYP of selected family planning methods
A 2011 study found that the service delivery cost per couple years of protection (CYP) for vasectomy was very low and roughly one-half that of tubal ligation.
9
Details


“For each method, the direct service delivery cost per CYP (not including facility overhead or demand creation activities) is calculated across USAID's 13 tier one family planning/reproductive health priority countries. The height of each bar shows the average value of the direct service delivery cost per CYP across the 13 USAID priority countries, while the height of the line represents the range of costs across these same countries. Data used to determine service delivery costs came from RH Interchange and UNFPA's RH costing model.”
More recent analyses in Haiti, Kenya, Uganda, Tanzania, and Rwanda show that contraceptive use is higher in areas where more methods are available.
A widely cited review by Ross & Stover found that making one additional contraceptive method available is significantly associated with increased contraceptive use.
11,12
Source: Track 20. (2017). Availability of methods.
In two-thirds of FP2030 countries, less than 30% of the population has access to vasectomy. Expanding access to vasectomy is necessary to ensure method choice.
4
Increasing choice
Access
Increasing access to vasectomy is critical to method choice
The global family planning community cannot achieve our goal of ensuring method choice if vasectomy remains widely unavailable



For example, in Haiti, the odds of women
using contraception is…

73%
higher
If they live near one facility offering three or more methods
From 1990 to 2019, the global contraceptive prevalence rate increased from 42% to 49%.
14
Demand for permanent methods
CPR growth
Demand for limiting births is high and likely to rise
In low- and middle-income countries, vasectomy is well-suited to meet the needs of those who do not wish to have any or more children
Sub-Saharan Africa
13% to 29%
Oceania
20% to 28%
Northern Africa
and Western Asia
26% to 34%
Central and Southern Asia
30% to 42%
Latin America
and the Caribbean
40% to 58%
From 1990 to 2019, contraceptive prevalence increased in all major geographic regions
Vasectomy has a very low risk of complications or side effects. While tubal ligation is also considered very safe, it requires:
Benefits
Safety
Vasectomy preserves women’s health and promotes gender equality
Investing in male-controlled contraceptive methods improves family planning and reproductive health outcomes and enables men to share responsibility for contraception
Gender equality
Public health impact
2
Women relying on their partner’s vasectomy to prevent pregnancy are well-protected, as vasectomy is one of the most effective contraceptive methods.
Though vasectomy is a male-controlled
method, it offers many benefits for women.
2,7



Scalpel incisions
A longer recovery time
General anesthesia, which carries greater risk
Annual probabilities of pregnancy with contraceptive methods
Like all contraceptive methods, vasectomy reduces the risk of maternal morbidity and mortality by averting risks associated with pregnancy, including unsafe abortion.
16,17
Source: Sonnenberg, F.A. et al. (2004). 69(6), 447-459.
7
Promote the role of men as caring partners by allowing them to share responsibility for contraception.
Reduce the contraceptive burden placed on females.
Challenge the notion that FP is a “women’s issue.”
Evidence shows that addressing gender by engaging men and boys in family planning programs can improve gender equality.
18,19
Specifically, increasing vasectomy uptake would
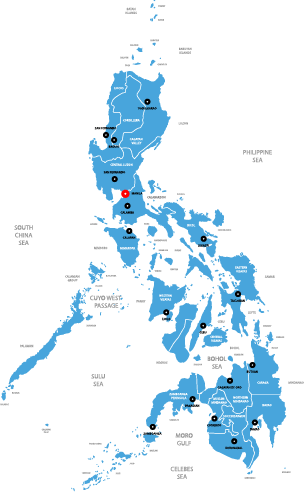
Cumulative public health impacts of a 5% increase in the use of vasectomy for limiting births (2016–2020)

Hover over pins
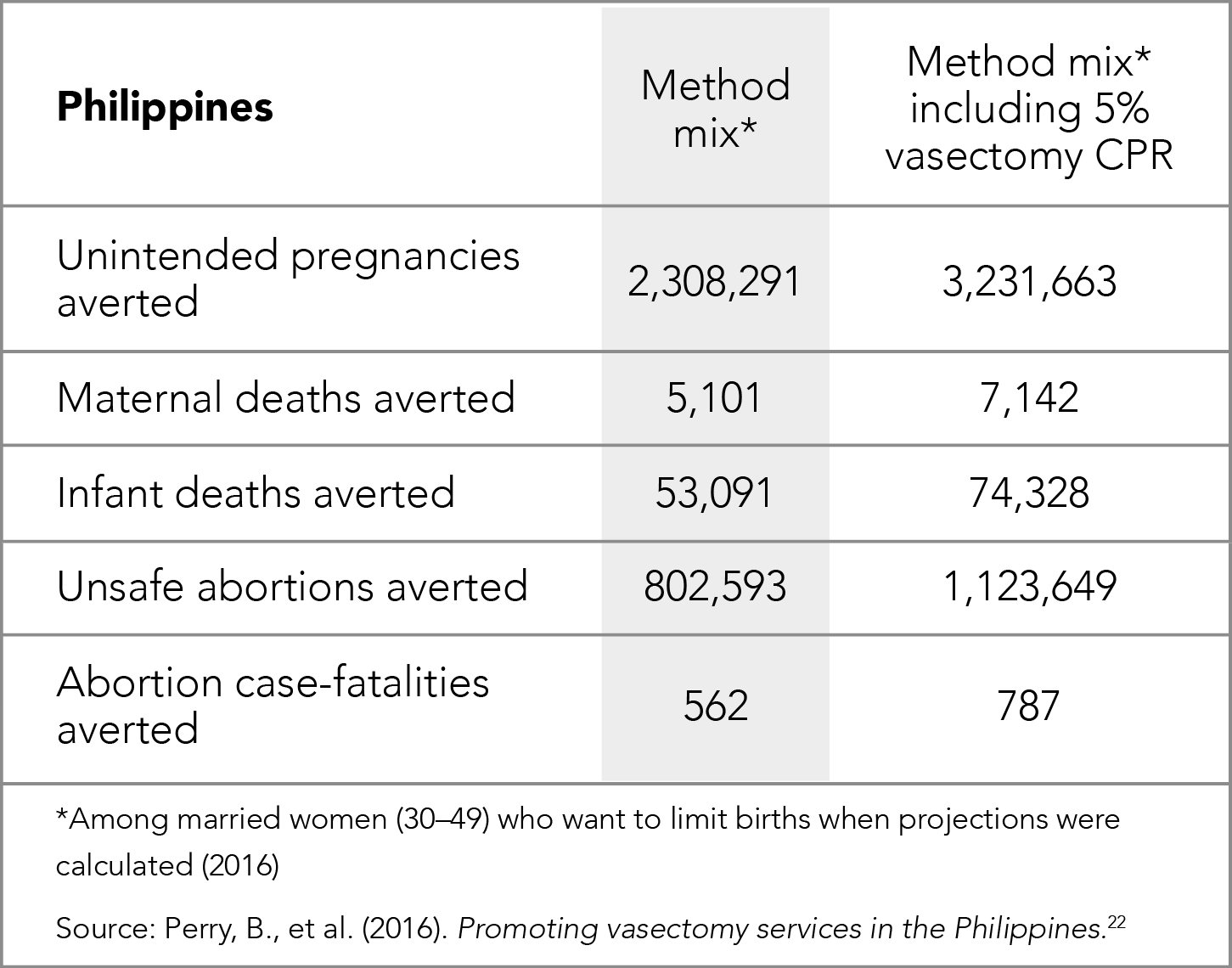


Philippines
Ghana
India
Global demand
Evidence shows we can increase the demand for vasectomy
Program designers and implementers can draw from existing evidence and materials to create effective vasectomy programs
Rwanda
Spotlight: Brazil
Key resources
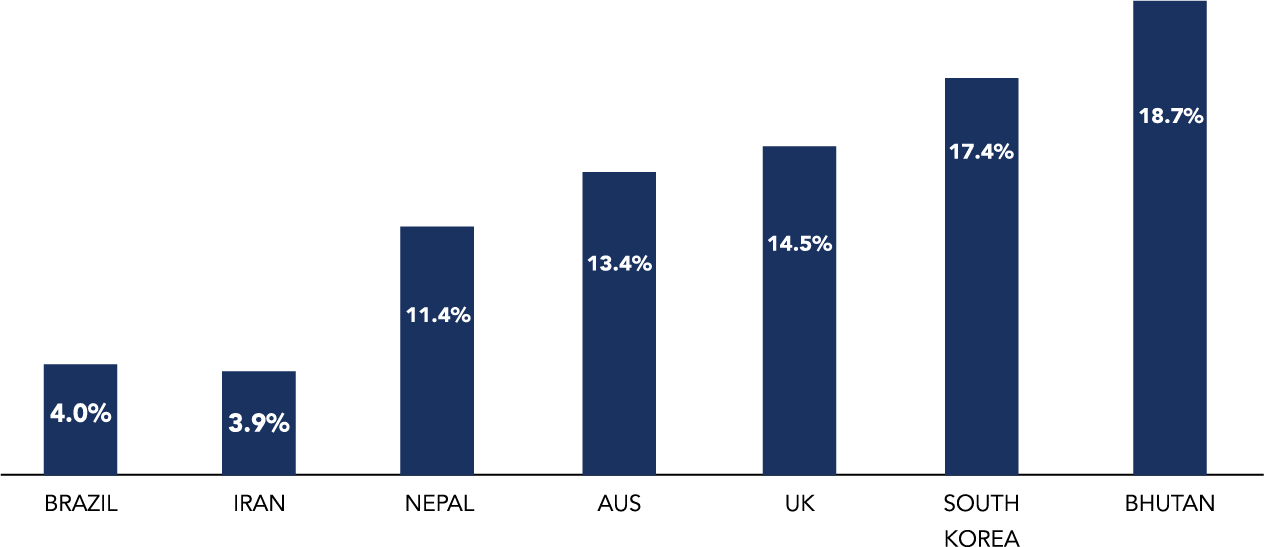
Evidence shows that over time, vasectomy can account for a large share of contraceptive use.
5,24
In India, the RESPOND Project increased intent to use long acting or permanent methods in the future by engaging men in the workplace.
More recently, The Challenge Initiative for Healthy Cities male engagement strategy saw an 87% increase in no-scalpel vasectomy in 20 cities between February 2019 and January 2020.
27
RESPOND Project vasectomy video
RESPOND Project vasectomy materials for India
26
Improved vasectomy knowledge
Increased acceptability of permanent methods
In the Philippines, group counseling sessions that promoted conversation about no-scalpel vasectomy:
28


A 300% increase in
non-scalpel vasectomy procedures
Increased proportion of men who said they would consider vasectomy
Improved health staff attitudes towards and knowledge about vasectomy
Results showed:
29
The ACQUIRE Project improved client and provider knowledge and acceptance of vasectomy in Ghana through provider training and targeted health promotion.
29,30
The PROGRESS Project successfully trained physicians to perform a new occlusion technique, which led the Ministry of Health to implement a country-wide training of doctors and nurses.
Over two years, this cascade training approach resulted in:
33
In Rwanda, the Capacity Project increased demand for vasectomy services so much that demand could not be met through a subsequent scale-up program.
32
additional
nurses trained
vasectomies performed
64
additional doctors trained
103
2,523
Brazil: Animated Vasectomy Hearts
Watch campaign video
Impact of a Mass Media Vasectomy Promotion Campaign in Brazil (Article)
Read now
The “Dancing Hearts” mass media campaign in Brazil (1989–1990) increased monthly mean number of vasectomies performed at three clinics during the campaign by:
25
in Fortaleza
108%
in São Paulo
82%
in Salvador
59%


Compared to an average of 310 per month before the campaign
Peaked at 689 vasectomies performed
Data from a clinic in São Paulo shows a dramatic increase in vasectomies immediately after the campaign:
25
Effect of a mass media campaign on the number of vasectomies performed per month at the PRO-PATER clinic in São Paulo (Poisson regression)
Jan
1988
Jan
1989
Jan
1990
Jan
1991
0
400
200
800
600
Vasectomies
Poisson model
1989 campaign
Number of vasectomies
Source: Kincaid, D.L., et al. (1996). Impact of a mass media vasectomy promotion campaign in Brazil.
25
Review of Lessons Learned in Vasectomy Programming (Report)
Read now
A Review of 10 Years of Vasectomy Programming (Article)
Read now
Vasectomy: A Long, Slow Haul to Successful Takeoff (Article)
Read now
Men as Contraceptive Users (Working Paper)
Read now
Expanding access to vasectomy sets the stage for future male method introduction new male methods in the future
Expanding access to vasectomy now will enable the family planning community to effectively support voluntary use of new male methods in the future.
New male contraceptives are in development, including an injection, implant, and more.
Generating demand for male methods.
The family planning community and country decision-makers need to invest in:
Creating an enabling environment for their use.
Download the full case study



Source: Track 20. (2017). Availability of methods.
Why do men and couples choose vasectomy?
Sub-Saharan Africa
3.9%
<0.1%
Source: United Nations, Department of Economic and Social Affairs, Population Division. (2019). Contraceptive Use by Method 2019.


2
1
3
Use of contraception continues to increase worldwide





How would increasing access to vasectomy improve method choice?
Percent of the population with access to vasectomy in FP2030 countries
Method choice is limited when vasectomy is inaccessible
Vasectomy has a very low service delivery cost per couple years of protection
"CYP is the estimated protection provided by contraceptive methods during a one-year period, based upon the volume of all contraceptives sold or distributed free of charge to clients during that period."
9
Vasectomy is underfunded
Vasectomy is underutilized
Vasectomy is unavailable







10
According to USAID, method choice exists when “client-centered information, counseling and services enable women, youth, men, and couples to decide and freely choose a contraceptive method that best meets their reproductive desires and lifestyle, while balancing other considerations important to method adoption, use, and change.”
Demographic trends indicate that demand for permanent methods is likely to grow
Past vasectomy programs
As of August 2020, Breakthrough ACTION was unable to identify any large-scale family planning programs with a focus on vasectomy.
The same review found only a small number of vasectomy initiatives tied to other funders.
6
If they live near more than one facility offering three or more methods

123%
higher



Vasectomy is safer and less invasive than tubal ligation
Vasectomy protects against unintended pregnancy and maternal morbidity and mortality
Increasing access to vasectomy would improve gender equality in family planning
The public health impact of the method mix would improve if even small numbers of women who want to limit births switched from shorter-term methods to relying on their partner’s vasectomy for contraception.
Increasing uptake of vasectomy would improve the public health impact of the method mix
Past programs have generated demand for vasectomy and delivered high-quality vasectomy services
India
Philippines
Ghana
Rwanda
Spotlight: The “Dancing Hearts” campaign increased vasectomy uptake in Brazil
Countries where vasectomy accounts for
a large share of contraceptive use

The Challenge Initiative male engagement strategy







Promising examples






Source: United Nations Department of Economic and Social Affairs, Population Division (2020). World Fertility and Family Planning 2020: Highlights.
Couples are having fewer children and ending childbearing at younger ages.
15
Demand to limit births exceeds demand to space among people of reproductive age in every region except West and Central Africa.
15
The average age at which the demand to limit exceeds the demand to space births is falling to as low as 23 or 24 in some countries.
15
Key Resources
Rwanda
Developing programming to reach individuals and couples with male contraceptive services.











Click on the icons below to learn more































Courtesy of Dominic Chavez/World Bank
1
4
5
9
9
4
13
7
20-23
Source: United Nations, Department of Economic and Social Affairs, Population Division. (2019). Contraceptive Use by Method 2019.
14
5
4
5


Courtesty of Alex Carrasco, licensed
under CC BY-NC-ND 3.0
Courtesy of Yagazie Emezi/Getty Images/Images
of Empowerment. Some rights reserved.


9
Source: Track 20. (2017). Availability of methods.
4
13
14
2
13
13
20-22
Source: United Nations, Department of Economic and Social Affairs, Population Division. (2019). Contraceptive Use by Method 2019.
5
How should I use it?
This tool is for anyone seeking to advocate for increased attention to vasectomy in family planning programs with key stakeholders in government, coordinating bodies, and funding organizations
Why men and couples choose vasectomy
The problem: Vasectomy is unavailable, underutilized, and underfunded
Why vasectomy should be included in family planning programs: Six key messages with supporting points and evidence
Two country case studies
Review the Vasectomy Message Framework to prepare for your advocacy conversation; select the key message most likely to persuade to your stakeholder.
HOW TO USE THIS TOOL
Why should I use it?
Persuade your stakeholder. Use the presentation content in this tool to advocate for vasectomy with your stakeholder, focusing on the key message you selected from the message framework.
Click here to jump to the presentation content for each of the six key messages.
Who is this for?
The presentation content covers:
Step 2
Step 1


The presentation content covers:
This tool provides compelling presentation materials that make it easy to advocate for vasectomy with key stakeholders.
31
31
32