Context
 A multitude of factors influence how health care providers deliver services. However, few provider initiatives have acknowledged and addressed the full range of interconnected factors, leading to persistent challenges in quality service delivery. To shift the narrative on provider behavior change, Breakthrough ACTION developed a groundbreaking set of tools:
A multitude of factors influence how health care providers deliver services. However, few provider initiatives have acknowledged and addressed the full range of interconnected factors, leading to persistent challenges in quality service delivery. To shift the narrative on provider behavior change, Breakthrough ACTION developed a groundbreaking set of tools:
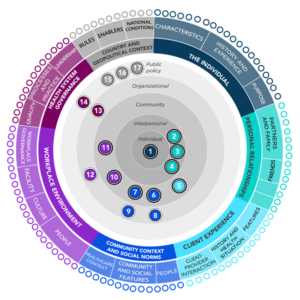
- The Provider Behavior Ecosystem Map
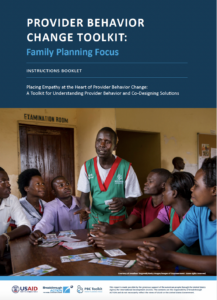
- Provider Behavior Change Toolkit for Family Planning
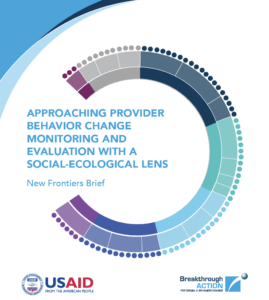
- Provider Behavior Change Monitoring and Evaluation Brief
The tools place the provider at the center and highlight the complex system of factors influencing providers. Used and adapted in over 10 countries and across multiple health areas, these tools help users consider what influences providers across the health system and then design, implement, and evaluate provider initiatives with that understanding.
“When I first saw the [Provider Behavior] Ecosystem Map, I thought, ‘Here’s something we’ve been missing. We’ve done a lot of training, a lot of supervision, the infrastructure—though insufficient—is there, but … these elements are not the only ones that determine the quality of reproductive health and family planning services.”
— Director of Mother and Child Health, Nursing and Obstetrics, Benin
Tool Overview
Provider Behavior Ecosystem Map
The Provider Behavior Ecosystem Map is an interactive map that highlights the many factors that influence facility-based providers and how those factors interact. Factors are organized into seven categories: (1) the individual provider, (2) personal relationships, (3) the client, (4) community context and social norms, (5) workplace environment, (6) health system governance, and (7) country and geopolitical context.
User Objectives
- Understand and consider diverse factors that influence facility-based provider behavior.
- Understand how factors relate to and interact with one another across a system.
- Think more holistically about provider-related health system strengthening efforts.
Priority Audiences
Social and behavior change; health systems strengthening; and service delivery practitioners, researchers, and donors.
Provider Behavior Change Toolkit for Family Planning
The Provider Behavior Change Toolkit for Family Planning guides users through a four-step human-centered design process to support provider behavior change. The toolkit positions providers as active participants in identifying challenges and developing solutions and collects data from multiple sources across the provider ecosystem.
User Objectives
- Identify, understand, and prioritize factors influencing provider behavior.
- Design and implement locally appropriate, supportive provider-related initiatives that address root causes of behavior.
Priority audiences
Social and behavior change and service delivery practitioners in coordination with facility-based providers and Ministry of Health representatives.
Approaching Provider Behavior Change Monitoring and Evaluation with a Socio-Ecological Lens (brief)
The Approaching Provider Behavior Change Monitoring and Evaluation with a Socio-Ecological Lens [brief] explores the current state of provider behavior change monitoring and evaluation efforts and provides recommendations for applying a systems lens to these efforts. The brief includes a list of commonly used data collection and analysis methods as well as a set of illustrative indicators for each level of the Provider Behavior Ecosystem.
User Objectives
- Understand gaps and challenges related to the current provider behavior change monitoring and evaluation efforts.
- Review examples of complexity-aware approaches, methods, indicators, and tools at each level of the Provider Behavior Ecosystem.
- Apply a socio-ecological lens to provider behavior change monitoring and evaluation efforts.
Priority audiences
Program planners, implementers, and researchers working at the intersection of health systems strengthening, service delivery, and social and behavior change or otherwise working to understand and improve provider behavior through PBC interventions.
These instructional videos provide more information on using the suite of PBC tools.
“By leveraging the PBE framework, stakeholders can foster an environment that not only enhances provider behavior but ultimately improves patient experiences and outcomes in health care settings.”
— User, India
Adaptations and Uses
Overview
 As of November 2024, the Provider Behavior Change tools have been used or adapted by at least ten projects or programs across ten countries, including those listed below.
As of November 2024, the Provider Behavior Change tools have been used or adapted by at least ten projects or programs across ten countries, including those listed below.
Provider Behavior Ecosystem Map (PBE Map)
- Used by the MOMENTUM Safe Surgery in Family Planning and Obstetrics (MSSFPO) team in India to identify the various interconnected factors influencing interpersonal communication behaviors among providers and as the framework for developing two provider behavior change tools on emergency obstetric care.
- Used by Breakthrough ACTION and the USAID Uzazi Staha (Respectful Maternity Care) project to understand provider behavior in the maternal and child health context and to inform their design of a compassionate care intervention in Tanzania.
- Used by the West Africa Breakthrough ACTION team to categorize and communicate their research findings on family planning quality service delivery challenges and provider needs in Burkina Faso, Côte d’Ivoire, Niger, and Togo.
- Used by the Breakthrough ACTION Sexual and Reproductive Health team to summarize literature review results on factors influencing community health workers globally compared to facility-based providers.
Provider Behavior Change Toolkit (PBC Toolkit)
- Adapted by MOMENTUM Integrated Health Resilience (MIHR) to suit the needs of providers and incorporate community health workers in Sudan and South Sudan.
- Tailored by the USAID SBCA team in Uganda to improve provider behavior and attitudes across family planning, maternal and child health, tuberculosis, and HIV.
- Adapted by Breakthrough ACTION staff in South Sudan to ensure cultural relevance and reflect the needs of an emerging health system.
- Used by Save the Children in Sierra Leone to address privacy concerns and improve family planning providers’ attitudes.
- Used by Pathfinder International’s Uganda Family Planning Activity to identify how provider behaviors were impacting family planning services uptake in Uganda.
- Adapted by MOMENTUM Country and Global Leadership for application to Integrated Management of Neonatal and Childhood Illness, shortening it to be used in half a day (awaiting testing in Zambia).
Use Case Snapshots
Uganda PBC Toolkit

Objectives and Methodology
Research indicated that provider attitudes and behaviors consistently negatively influenced family planning service uptake in Uganda. To improve client-centered family planning service provision and address discrimination toward youth, the USAID Social and Behavior Change Activity (SBCA) Uganda project implemented the PBC Toolkit in eight districts. In collaboration with the Ministry of Health, SBCA first pretested the PBC Toolkit and held an adaptation workshop to contextualize the tools. This resulted in adding other health content (maternal health, HIV, and tuberculosis), shortening some tools, tailoring client scenarios and images, and simplifying questions. The toolkit data collection process uncovered multiple factors influencing providers, from poor feedback mechanisms to community norms, supply chain disruptions, and lack of motivation. Providers, community members, and health management brainstormed and implemented initiatives to address prioritized factors, including streamlined communication systems, reward programs, and creating mental health committees.
Results
- Findings revealed improved communication between health workers and clients.
- Providers reported improved working relationships between providers in their workplaces.
- The collaborative process employed by the PBC Toolkit improved feedback mechanisms between the district health teams and providers.
Adapted Tool
Uganda Provider Behavior Change Toolkit
South Sudan PBC Toolkit
Country: South Sudan
Objectives and Methodology
Breakthrough ACTION staff in South Sudan wanted to align provider behavior with clients’ reproductive intentions and fertility desires. To do so, they knew they needed to better understand and address the factors influencing providers in South Sudan. To reflect the realities of providers in a young country with an evolving health system, they adapted and tailored the PBC Toolkit. Using findings from advanced audience segmentation research and input from stakeholders in a co-design adaptation workshop, they added South Sudan-specific client and provider profiles, incorporated new influence factors relevant to the context—including willingness to discuss sensitive topics, the need for partner consent, and youth-specific expectations—and pre-populated examples to demonstrate how to analyze results. They also ensured all imagery, language, and framing resonated with their broader campaign and the country context so that other partners could implement the toolkit.
Results
- The PBC Toolkit enabled localized understanding of providers’ needs by highlighting norms and factors influencing providers in South Sudan.
- Pretesters indicated the adapted Toolkit could help them customize interventions.
“This tool is practical and relevant, truly addressing the behaviors that matter most for supporting reproductive health.” — Implementer, South Sudan - The toolkit sparked collaboration and new thinking.
“[The toolkit] helps in igniting thinking around activities, coordination, challenges, and opportunities for providing better health services.” — State Ministry of Health, Yambio, South Sudan
Adapted Tool
Tanzania Compassionate Care Provider Behavior Ecosystem
 Country: Tanzania
Country: Tanzania
Objectives and Methodology
Breakthrough ACTION, together with the USAID Uzazi Staha project, aimed to increase compassionate care during an extended postpartum period (one year post birth) in Tanzania. They examined the domains in the original PBE Map and reviewed the literature to identify factors that influenced maternal, newborn, and child health (MNCH) health providers and services. Using the PBE Map as a framework, they summarized the key influencing factors and then employed a human-centered design process to co-design an intervention for facility-based providers. The resulting compassionate care intervention deliberately addressed multiple levels and factors from the PBE Map.
Results
- “Using the PBE Map to explore the most pressing factors at play in a given facility or service helped us think more comprehensively about how best to solve for the challenge at hand and improve service quality. It pushed us to consider factors that would have otherwise been overlooked and helped us focus in on workplace culture and power rather than immediately thinking that more training was needed.” — Core design team member, Tanzania; emphasis added
- The review of the MNCH literature validated the PBE as a conceptual framework and confirmed that many factors outlined in the PBE are relevant to other health areas.
- Post-intervention, participating facilities reported a statistically significant increase in their perception of support from their health facility across six components including agreeing that help is available from the facility when they have a problem or that the facility really cares about their wellbeing, among others.
- Improvements among providers appear to have led to improvements in experience of care for clients. Clients reported vast improvements in the intervention facilities across all 10 of the metrics tested, with all highly statistically significant.
Adapted Tools
Sudan and South Sudan PBC Toolkit
Countries: Sudan and South Sudan
Objectives and Methodology
Sudan and South Sudan face unique challenges related to service delivery due to their fragility. Desiring to improve the quality of family planning services and recognizing the many factors affecting provider behavior, MIHR adapted the PBC Toolkit for use in both countries. MIHR tailored the content and structure for fragile settings and contextualized and simplified the tools. Additionally, MIHR developed a comprehensive package to facilitate the toolkit’s use, including a roadmap, a seven-part video series, and training agendas. To measure changes in provider behavior, before implementing the PBC Toolkit, MIHR conducted a baseline using the Provider Authoritarian Attitudes Scale, which will be repeated after six months of implementation.
Results
- The toolkit enabled practitioners to identify many factors they had not previously considered as influencing family planning providers, from attitudes to health facility administration to community norms.
- “The concept of [the ecosystem] makes a lot of sense to us, especially in Bor where there are lots of social norms that hinder the uptake of services.” — Doctor, South Sudan
- Using the toolkit raised political awareness of provider needs, which facilitated enhancements to facilities such as chairs and tables for triage and registration, new tools, and sanitizing equipment.
Adapted Tool
Sudan and South Sudan Provider Behavior Change Toolkit Package
Lessons Learned
 Advocating for providers is more effective when stakeholders understand the tools’ purpose and are engaged from the beginning. It is critical to involve key stakeholders like District Health Teams and facility managers from the beginning, and throughout the process. They must understand and buy into the PBC Toolkit to facilitate the data collection and brainstorming processes. Stakeholders who see the value of the tools and understand providers’ realities are more likely to advocate for resources to address challenges and fund solutions that arise from the toolkit process.
Advocating for providers is more effective when stakeholders understand the tools’ purpose and are engaged from the beginning. It is critical to involve key stakeholders like District Health Teams and facility managers from the beginning, and throughout the process. They must understand and buy into the PBC Toolkit to facilitate the data collection and brainstorming processes. Stakeholders who see the value of the tools and understand providers’ realities are more likely to advocate for resources to address challenges and fund solutions that arise from the toolkit process.- Investing the time required to unpack, adapt, and implement is worthwhile. The PBC Toolkit requires careful exploration of factors at multiple levels and involvement of diverse actors to get a holistic view of provider behavior. Unpacking the complexity of provider behavior, along with adapting the tools to uncover quality insights, is an investment, but it is worth the time spent.
“Taking the extra time allowed us to develop tools that were more relevant and practical for the local context. Adapting tools to fit the realities on the ground, even if time-consuming, leads to more meaningful and sustainable impact in the long run.” — Implementer, South Sudan - Involving providers meaningfully requires accommodating their busy schedules. Engaging providers in the identification of challenges and solutions enhances relevance and acceptance. However, providers are busy professionals, and it can be difficult to find adequate time to involve them in this process. Some users found that engaging providers during their work hours compromised the quality of insights provided. Working with facility managers to clear provider schedules and asking providers when they prefer to be involved helps them fully participate.
- Keeping an open mind about what influences provider behavior and how to address them is essential to understanding providers’ reality. When using the Ecosystem Map and PBC Toolkit, it is important to ask questions with humility and set aside assumptions to enable the exploration of all potential factors. Similarly, being open to new ways of resolving persistent challenges—including looking for strengths and solutions that providers already employ—improves the quality of solutions.
- Building trust with providers and stakeholders is essential to effective implementation. Providers often feel blamed during improvement processes. For the PBC Toolkit to be effective, implementers must build trust with providers, explaining its purpose and emphasizing its supportive, solutions-focused nature. If providers view the process as investigative, they may hold back information or ideas. Similarly, building trust and seeking solutions with District Health Teams and facility managers facilitates use of the toolkit and implementation of new ideas.
- Distributing responsibilities and costs among implementing partners makes the process more sustainable. Carrying out the PBC Toolkit and implementing solutions from the process requires resource and time commitment. Ideally, these should be shared across the partners involved in its implementation to increase effectiveness and sustainability. The groups involved in implementing the toolkit also need to agree upon action items post-implementation.
- Creating and using supportive materials can enhance understanding of the tools. Implementers found it can be helpful to provide supplemental materials, such as the roadmap and video series MIHR created. These materials allow implementers to see practical applications of the toolkit and provide a clear process for carrying out the activities.
Good Practices
 Tailor to the local context. Begin by pretesting the PBC Tools to determine cultural relevance and needed adjustments. Engage local stakeholders in the process of adapting the tools, ensuring that changes are grounded in evidence and aligned with the realities of the context where the tools are being used. Identify words and images that are understandable and relatable to the providers, clients, and other stakeholders involved. Continuously gather feedback on the tools to enable real-time adjustments that keep the tools practical.
Tailor to the local context. Begin by pretesting the PBC Tools to determine cultural relevance and needed adjustments. Engage local stakeholders in the process of adapting the tools, ensuring that changes are grounded in evidence and aligned with the realities of the context where the tools are being used. Identify words and images that are understandable and relatable to the providers, clients, and other stakeholders involved. Continuously gather feedback on the tools to enable real-time adjustments that keep the tools practical.- Prioritize buy-in. Engage a diverse group of stakeholders early on, helping them feel invested in supporting providers. Clearly explain the systemic, supportive approach and model empathy toward providers. Support these stakeholders to be champions, advocating for these approaches and tools in their networks as well as funding to support provider-supportive initiatives.
- Accommodate stakeholder schedules. Determine the most appropriate time to engage providers and clients, acknowledging their busy schedules. Improve the quality of insights by reducing stressors and meeting participants where they are.
- Keep it simple. Simplify complex concepts and content so it resonates with participants. Identify which materials and tools will be most useful in the local context and prioritize those. Use a roadmap or other visual aids that help participants understand the purpose and flow of the tools.