Voices from the Front Lines: Breakthrough ACTION Responds to Ebola in Guinea
Written by: Antonia Morzenti, Breakthrough ACTION Program Officer
Ebola virus is deadly: the survival rate, depending on the strain, can be as low as 10%, and death can happen sometimes in as little as six days. For Ebola patients and those in their community, this is very sobering news.
For a disease like Ebola, time saved equals lives saved. When Ebola struck Guinea in February 2021, Breakthrough ACTION immediately responded with one of the most powerful tools: prior experience. Specifically, the project tapped into Johns Hopkins Center for Communication Program’s experience with the 2014 Ebola outbreak response and Breakthrough ACTION’s COVID-19 response work in Guinea.
 To capture the experiences and lessons learned from the front lines, Breakthrough ACTION’S Antonia Morzenti, Program Officer, spoke with three team members in Guinea: Amiata Kaba, Program Manager; Fatoumata Hann, Program Assistant; and Charles Loty, Ebola Advisor.
To capture the experiences and lessons learned from the front lines, Breakthrough ACTION’S Antonia Morzenti, Program Officer, spoke with three team members in Guinea: Amiata Kaba, Program Manager; Fatoumata Hann, Program Assistant; and Charles Loty, Ebola Advisor.
This is what they had to say (translated from French):
Antonia Morzenti (AM): As you probably remember, Guinea declared itself Ebola-free in June 2016 after the first Ebola outbreak of 2014. What were your first thoughts when you found out that Ebola was back again?

Amiata Kaba
Amiata Kaba (AK): It was a surprise to me. I found out about the new outbreak on TV, and I thought, “How is Guinea going to react to this outbreak?” Then I thought about what the reactions of the population, the citizens, and the community would be. What are we going to do with the stigma associated with Ebola? Then I thought about the resources we would need to battle against a pandemic [COVID-19] and an Ebola outbreak at the same time.
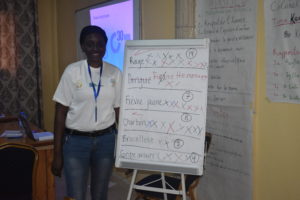
Fatoumata Hann
Fatoumata Hann (FH): My first thoughts were, “We are in a bad situation! Not only are we in a pandemic [COVID-19], but we now also have Ebola. This mix is going to be very complicated!” I knew that we needed to make sure people understand that Ebola was something real.
Charles Loty (CL): Astonished. I couldn’t believe Ebola was back. Then, I thought about the weak public health systems we have.
AM: What do you feel has been the biggest challenge in the Ebola response?
AK: We have many different challenges, but the most critical one is that we need to constantly improve and perform well. We have to be efficient, and we need to continue on that path.
FH: The biggest challenge is trust. The community does not trust the government and its messages.
CL: The biggest challenge is changing the population’s perception of the severity of the epidemic. We need to strengthen communication activities through community dialogues, focus groups, and community debates in the communities by involving local leaders.

Antonia Morzenti
AM: What are you currently doing to address these challenges?
AK: We are thinking and working on our interventions I am always listening so that we can improve our risk communication and community engagement actions and listening because everything is constantly changing in this epidemic.
FH: We need to get together with people we know and partners that can help us.

Charles Loty
CL: We are working to prevent and address the spread of rumors, misinformation, and disinformation about Ebola. We are also sharing practical advice with partners on activities directly related to the development or implementation of plans and strategies. We are also engaging with the media at the prefectural level to encourage responsible reporting and to share key health information so that we can combat the spread of rumors and misinformation.
AM: Breakthrough ACTION is always working to innovate and advance the field of social and behavior change (SBC). Based on your Ebola response work, what are some lessons learned you would like to share with the global SBC community?
AK: The first lesson learned is that we need to have a plan—pre-epidemic—that can be adapted for any phase of the epidemic. We need a plan that can be put in place fast; what are the activities that we can implement immediately? Another one is that we need to adapt to the social and cultural contexts. We need to be able to rapidly scan the global and community landscapes so we know which are the strengths and which are the challenges we might have; we need to see what we have and what we can do. Next, we need to put in place a partnership framework for our response efforts. We need to know who the actors are and we need to be partners and coordinate with them. At the beginning of the epidemic, many organizations and people came to Nzérékoré. Each actor brought its unique approach. We need to integrate and manage different approaches. Together, we can create the “force” that is required for this response work.
FH: To get a good response, we need to engage with the community. We need to include them before we establish our strategy. We need to construct together.
CL: We need to understand the different characteristics of the disease and how we—Guineans—can protect ourselves. Then we need to establish a communication strategy. We need to have the support of national organizations and we need to reinforce community engagement, every day.
AM: What do you think is the most important thing to do or has to happen for Guinea to become and stay Ebola-free?
AK: First, we need to reinforce our alert system within the community. With a community system, people can report when they see something unusual, allowing us to intervene quickly. In this way, communities can conduct their own surveillance. They need to be in control of and follow up on this epidemic. Second, we need a continued system of education. We need to reinforce the population’s comprehension of the risk of zoonotic disease and community health workers need to be trained and prepared to signal alerts when necessary. Third, we need to promote public health at all levels in Guinea. Finally, we must integrate human health, animal health, and environmental health.
FH: We need to continue with prevention. Prevention and action.
CL: Health systems need to be reinforced. We also need better research.
AM: If you have to describe Breakthrough ACTION’s Ebola response work in one word, what would that be?
AK: It would have to be “resilient” because we need to continuously reflect on new solutions and new approaches, and we need to introduce new innovations. We also need to be resilient with our collaboration with different partners.
FH: Efficient.
CL: Since we are in the field of communications, [the word] would be CLEBA: Communication pour la Lutte contre Ebola Breakthrough ACTION (Communication for the Fight Against Ebola with Breakthrough ACTION).
AM: Thank you all for your time!

 UNICEF Guinea
UNICEF Guinea Gopal Bhattacharjee/Photoshare
Gopal Bhattacharjee/Photoshare Poravute/Getty Images
Poravute/Getty Images Sean Maloney/Breakthough ACTION
Sean Maloney/Breakthough ACTION Anne Ballard Sara/Breakthrough ACTION
Anne Ballard Sara/Breakthrough ACTION K4Health
K4Health